Comprehensive Cardiology Seminar and Board Review Course
Release Date: 11/1/2015
Target Audience
- Practicing cardiologists seeking continuing medical education and knowledge update
- Practicing cardiologists preparing for Board Certification or Recertification
- Fellows preparing for the Board Certification Examination
Course Description
The NYU Comprehensive Cardiology Seminar and Board Review provides an intensive and comprehensive review of cardiovascular medicine. The program focuses on current guidelines and appropriate use criteria in general clinical cardiology, clinical cardiac electrophysiology, invasive cardiology, cardiovascular prevention and cardiovascular genetics. In addition to thematic lectures, the program includes review sessions, case-based questions and review of images in cardiology and electrocardiograms. The program also includes presentations on changes in the health-care system and their potential impact on the practice of evidence-based quality cardiovascular medicine. This course is of particular value to those preparing for the Board Certification exam. There is supplementary content that includes practice sessions on test-taking skills and review of images in cardiology and electrocardiograms similar to the materials tested on the board examination. A full-range of educational tools, including self-assessment activities, are embedded within the didactic lectures. Sample multiple choice questions are included in each presentation to help participants assess their own knowledge and assist those in preparing for their board exam.
Statement of Need
Progress in interventional cardiology technology and technique has rapidly accelerated in recent years. Depending on the training and skill of the cardiologist, as well as the quality of available imaging and catheterization equipment, the quality of care for patients with structural heart diseases can vary markedly. Paradoxically, the very rapid advances in technology that make interventional cardiology an increasingly effective subspecialty creates an inherent gap in knowledge for practicing cardiologists. There is a need to close this gap in quality cardiovascular disease management so that interventions that represent state of the art care are implemented. Management of heart failure requires a multimodal approach. It involves a combination of lifestyle modifications, medications, and possibly the use of devices or surgery. There is significant evidence of a practice gap in the treatment of congestive heart failure, particularly the underuse of β-blockers and aldosterone antagonists which have been shown to provide mortality benefit. The science of arrhythmia is central to cardiology. Atrial fibrillation is the most common form of arrhythmia. About 2.5 million Americans have atrial fibrillation. As the population ages, it is becoming more common: 2 to 3 percent of 60-year-olds have atrial fibrillation, but the rate rises to 12 percent for 80-year-olds. Once viewed as a nuisance, not necessarily something that required aggressive intervention, atrial fibrillation is now seen as a major risk factor for stroke and clear atrial fibrillation plays a role in stroke and a quality-of-life problem. Medication has long been the mainstay of treatment for atrial fibrillation; however, several studies show its effectiveness is limited. Cardiologists now perform surgical ablations where the errant electrical signals originate. There are different ablation techniques being used and there is a need to recognize the comparative effectiveness and the risks possible with each approach. There is also a need for clinicians to be better able to evaluate clinical situations where ablation may be a first-line treatment for atrial fibrillation rather than an option for patients who don’t improve after drug therapy. Proper selection of noninvasive testing remains a constantly evolving field. Newer types of tests are constantly being introduced into the field, creating a gap in the clinical practice of many cardiologists.
Clinicians need to be updated on these newer diagnostic tools and find the proper clinical situations for their use. Prevention of cardiovascular disease is one of the major accomplishments of the past sixty years. The use of lipid lowering and antihypertensive medications has proven to be highly effective. To prevent stroke, doctors often prescribe a range of blood thinners. There are considerable differences in the clinical effects of each class of drugs, based on their mechanism of action. Cardiologists need to be expert in the development of effective treatment regimens. This expertise derives from a comprehensive knowledge of clinical trial results as well as an understanding of the design of these studies and the variables they address.
Educational Objectives
After participating in this activity, clinicians should be able to:
- Outline updated guidelines relative to interventional cardiology
- Describe the latest technological advances in interventional cardiology and implement appropriately to optimize patient outcomes
- Evaluate newer medications to treat CHF and prescribe appropriately to ensure patient safety
- Review the currently available options of therapy and utilize newer modalities, such as ablation, atrial closure devices and newer anticoagulation regimens for optimal patient outcomes
- Evaluate the newer noninvasive tests available to diagnose and prognosticate patients
- Describe the clinical effects of each class of anticoagulants and prescribe appropriately to prevent stroke or minimize untoward outcomes
Program Topics
Introduction to the Certifying Examination — Format, Questions, Relevance, Test Taking Tricks
Steven M. Kobren, MD
Cardiovascular Physical Examination
Steven M. Kobren, MD
Cardiovascular Physiology
Adam Skolnick, MD
Peripheral Arterial Disease — Part 1
Michael J. Attubato, MD
Biostatistics — How Do We Interpret the Literature?
Harmony Reynolds, MD
Anticoagulation and Antiplatelet Therapy — Working Through the Maze
Jeffrey S. Berger, MD, MS
Chronic Coronary Artery Disease Management— State of the Art Management
Sripal Bangalore, MD, MHA
Genetics and Heart Disease
Glenn I. Fishman, MD
Pericardial Disease
Muhamed Saric, MD, PhD, MPA
Diastolic Dysfunction — Diagnosis and Management
Muhamed Saric, MD, PhD, MPA
Hypertension and Renovascular Disease
Arthur Z. Schwartzbard, MD
Hemodynamics in the Catheterization Laboratory
James Slater, MD
EKGs — What You Need to Know for the Boards
Jeffrey Lorin, MD
Questions — Board Type Questions with Detailed Answers
John T. Coppola, MD, MS
Cardiomyopathy — Trends in Diagnosis and Management
Mark V. Sherrid, MD
Ventricular Remodeling — Mechanisms and Management
Stuart D. Katz, MD
Systolic Dysfunction
Stuart D. Katz, MD
Advanced Heart Failure — Device Therapy, Surgery, Transplant
Alex Reyentovich, MD
Pulmonary Hypertension
Alex Reyentovich, MD
Peripheral Arterial Disease — Part 2
Michael J. Attubato, MD
Coronary Physiology and Endothelial Function
Steven P. Sedlis, MD
Emergency Cardiac Care
Robert O. Roswell, MD
Non-Invasive Testing — Who, Why and Which Test?
Lawrence Phillips, MD
Revascularization — Role of Invasive Testing and What Do We Do with the Results
John T. Coppola, MD, MS
Primary and Secondary Prevention of Cardiovascular Disease
Howard S. Weintraub, MD
Venous Thromboembolic and Lymphatic Disease
Ricardo J. Benenstein, MD
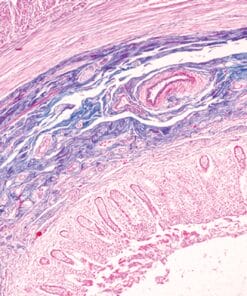
Images – Review of Images Likely to Appear on the Boards
John T. Coppola, MD, MS, and Robert Donnino, MD
Questions — Board Type Questions with Detailed Answers
John T. Coppola, MD, MS
ACS Management
Norma M. Keller, MD
NSTEMI — Diagnosis and Management
Jeffrey S. Berger, MD, MS
Reperfusion Strategies — Who Gets What
Louai Razzouk, MD, MPH
STEMI — Diagnosis and Management
Judith S. Hochman, MD
Aortic Insufficiency and Aortic Stenosis
Barry P. Rosenzweig, MD
Mitral Regurgitation and Mitral Stenosis
Barry P. Rosenzweig, MD
Valvular Hemodynamics — Review of Echocardiographic Evaluation
Muhamed Saric, MD, PhD, MPA
Prosthetic Heart Valves
Muhamed Saric, MD, PhD, MPA
Congenital Heart Disease for the Boards
Catherine R. Weinberg, MD
Electrophysiology and Drug Therapy
David S. Park, MD, PhD
Intracardiac Electrocardiograms — How do we Read Them and What Do They Mean?
David S. Park, MD, PhD
Mini Board Examination — Q & A Panel Discussion
Steven M. Kobren, MD
Channelopathies — Clinical Relevance for the Boards
Steven J. Fowler, MD
Pacemakers — Patient Selection and Evaluation of the Device
Charles J. Love, MD
Atrial Arrhythmias
Douglas S. Holmes, MD
Atrial Fibrillation
Larry A. Chinitz, MD
Ventricular Arrhythmia
Larry A. Chinitz, MD
ICD Device Therapy — Patient Selection and Evaluation of the Device
Charles J. Love, MD
Syncope — Guideline Based Evaluation and Management
William R. Slater, MD
Infective Endocarditis
Barry P. Rosenzweig, MD
Pre-Op and Management of Cardiac Patients for Non-Cardiac Surgery
William R. Slater, MD
Diabetes and The Heart
Howard S. Weintraub, MD
Pregnancy and Heart Disease
Catherine R. Weinberg, MD
Expert Faculty
COURSE DIRECTORS:
John T. Coppola, MD, MS
Clinical Assistant Professor of Medicine
Glenn I. Fishman, MD
William Goldring Professor of Medicine and Professor of Neuroscience, Physiology, Biochemistry and Molecular Pharmacology
Steven M. Kobren, MD
Clinical Associate Professor of Medicine
FACULTY:
Michael J. Attubato, MD
Associate Professor of Medicine
Sripal Bangalore, MD, MHA
Associate Professor of Medicine
Ricardo J. Benenstein, MD
Assistant Professor of Medicine
Jeffrey S. Berger, MD, MS
Associate Professor of Medicine and Surgery
Larry A. Chinitz, MD
Benjamin and Kenneth Coyle, Sr. Family Professor of Medicine and Cardiac Electrophysiology
Robert Donnino, MD
Assistant Professor of Medicine and Radiology
Steven J. Fowler, MD
Assistant Professor of Medicine
Judith S. Hochman, MD
Harold Snyder Family Professor of Medicine
Douglas S. Holmes, MD
Assistant Professor of Medicine
Stuart D. Katz, MD
Helen L. and Martin S. Kimmel Professor of Advanced Cardiac Therapeutics
Norma M. Keller, MD
Assistant Professor of Medicine
Jeffrey Lorin, MD
Assistant Professor of Medicine
Charles J. Love, MD
Professor of Medicine
David S. Park, MD, PhD
Assistant Professor of Medicine
Lawrence Phillips, MD
Assistant Professor of Medicine
Louai Razzouk, MD, MPH
Instructor of Medicine
Alex Reyentovich, MD
Assistant Professor of Medicine
Harmony Reynolds, MD
Saul J. Farber Assistant Professor of Medicine
Barry P. Rosenzweig, MD
Associate Professor of Medicine
Robert O. Roswell, MD
Assistant Professor of Medicine
Muhamed Saric, MD, PhD, MPA
Associate Professor of Medicine
Arthur Z. Schwartzbard, MD
Assistant Professor of Medicine
Steven P. Sedlis, MD
Associate Professor of Medicine
Mark V. Sherrid, MD
Professor of Medicine
Adam Skolnick, MD
Associate Professor of Medicine
James Slater, MD
The Robert and Marc Bell Professor of Cardiology
William R. Slater, MD
Associate Professor of Medicine
Catherine R. Weinberg, MD
Clinical Instructor of Medicine
Howard S. Weintraub, MD
Clinical Professor of Medicine
Accreditation Statement
The NYU Post-Graduate Medical School is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
TOTAL FILE SIZE: 28.5GB (PDF Syllabus + 51 Videos)