Course Description
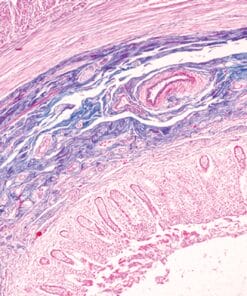
Frozen section diagnosis can be challenging, particularly when the pathologist is handling the case alone. This difficulty may be compounded by dramatic and irreversible surgical implications. Frozen section interpretation is totally based on the histologic features since ancillary testing, including immunohistochemistry and molecular studies are not available. Time is crucial to make a confident diagnosis because the patient is on the operating table under general anesthesia, and the surgeon needs to know a specific answer to make a decision on the subsequent procedure. This is one of the times that a pathologist guides the hands of a surgeon.The intra-operative consultation service is a critical component of a hospital-based pathology practice; it involves every sub-specialty surgery and almost every organ/system. A solid general pathology foundation is essential; keeping updated on new entities is extremely valuable.
Although books and chapters on frozen section diagnosis are available, organized lectures are rarely focused on frozen section diagnostic skills and pitfalls, particularly in the molecular era. Intimate mentoring around the microscope mimicking real time frozen section analysis has not been previously used.
This course addresses diagnosis under pressure and provides practicing pathologists and pathologists-in-training with guidance on how to handle diagnostic dilemmas on the frozen section service, avoid equivocation and effectively communicate with surgeons.
Target Audience
Practicing academic and community pathologists, and pathologists-in-training
Learning Objectives
Upon completion of this educational activity, learners will be able to:
- Understand the common clinical scenarios and indications that frozen section diagnoses aid in determining the surgical procedure.
- Become familiar with the common and critical artifacts to avoid misinterpretation.
- Improve diagnostic skills during the frozen section procedure with enhanced confidence, competence and efficiency, thereby reducing turn-around-time.
- Understand that deferral is a valid option to avoid uncertain interpretation and potential errors.
- Enhance communication with the operating surgeon, particularly when the histomorphology is uncertain, and there is potential for harmful error.
Continuing Medical Education and Continuing Certification
The United States and Canadian Academy of Pathology is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The United States and Canadian Academy of Pathology designates this enduring material for a maximum of 18.25 AMA PRA Category 1 CreditsTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
USCAP is approved by the American Board of Pathology (ABPath) to offer Self-Assessment credits (SAMs) and Lifelong Learning (Part II) credit for the purpose of meeting the ABPath requirements for Continuing Certification (CC). Registrants must take and pass the post-test in order to claim SAMs credit. Physicians can earn a maximum of 18.25 SAM/Part II credit hours.
Disclosures
The faculty, committee members, and staff who are in position to control the content of this activity are required to disclose to USCAP and to learners any relevant financial relationship(s) of the individual or spouse/partner that have occurred within the last 12 months with any commercial interest(s) whose products or services are related to the CME content. USCAP has reviewed all disclosures and resolved or managed all identified conflicts of interest, as applicable.
The following faculty reported no relevant financial relationships: Gregory Fuller, MD, PhD, John A. Hart, MD, Pei Hui, MD, PhD, Peter Humphrey, MD, Cesar Moran, MD, Jim Zhai, MD
The following IM Coordinator who planned and reviewed content for this activity reported no relevant financial relationships: Steven D. Billings, MD
USCAP staff associated with the development of content for this activity reported no relevant financial relationships.
Topics/Speaker:
Intraoperative Diagnostic Issues in GI Pathology Part 1
Intraoperative Diagnostic Issues in GI Pathology Part 2
Intraoperative Diagnostic Issues in GU Pathology Part 1
Intraoperative Diagnostic Issues in GU Pathology Part 2
Intraoperative Diagnostic Issues in GYN Pathology Part 1
Intraoperative Diagnostic Issues in GYN Pathology Part 2
Intraoperative Diagnostic Issues in Head and Neck Pathology Part 1
Intraoperative Diagnostic Issues in Head and Neck Pathology Part 2
Intraoperative Diagnostic Issues in Neuropathology Part 1
Intraoperative Diagnostic Issues in Neuropathology Part 2
Intraoperative Diagnostic Issues in Thoracic Pathology Part 1
Intraoperative Diagnostic Issues in Thoracic Pathology Part 2
Original release date: January 29, 2020
Access to this course expires on: October 4, 2022