Medical Ebook Review
Fundamentals of Implant Dentistry 2024: Essential Guide for Practitioners and Students
In the world of dentistry, dental implants have transformed the way practitioners approach tooth replacement. The fundamentals of implant dentistry 2024 not only reflect advancements in technology but also encompass an evolving understanding of patient needs and the complexities of oral rehabilitation. This comprehensive guide explores essential aspects of modern implant dentistry, providing insights that will enhance knowledge for both dental professionals and patients alike.
Introduction to Modern Implant Dentistry
Modern implant dentistry has become a critical component of restorative dentistry, offering patients a reliable solution for missing teeth. As we venture into 2024, it is crucial to examine how the field has evolved, focusing on the principles of successful implant placement, patient assessment, surgical techniques, and technological advancements. Understanding these fundamental elements will empower dental professionals to deliver excellent care, ensuring optimal outcomes for their patients.
The following sections will delve into various dimensions of implant dentistry, including historical context, anatomical considerations, treatment planning, material selection, surgical protocols, prosthetic options, and future trends. With this comprehensive guide, readers will gain a deeper appreciation of what makes implant dentistry a cornerstone of contemporary oral health care.
The Evolution of Dental Implants: From Ancient Times to 2024

The journey of dental implants stretches back thousands of years, showcasing humanity’s persistent quest for effective solutions to tooth loss. This section will highlight the significant milestones in the evolution of implant technology, culminating in the cutting-edge practices of 2024.
Historical overview of dental implants
The use of dental implants can be traced back to ancient civilizations. Archaeological findings suggest that the Mayans, Egyptians, and even Romans utilized rudimentary forms of implants made from materials such as wood, ivory, and metal. These early attempts at tooth replacement reveal the age-old desire for aesthetic and functional restoration.
In the mid-20th century, the field experienced a monumental shift with the discovery of osseointegration by Dr. Per-Ingvar Brånemark. His pioneering research laid the foundation for titanium implants, which are now considered the gold standard in dental implantology. The introduction of intraoral radiography and improved surgical techniques further propelled the field forward.
Today, advancements in materials science, digital technologies, and surgical protocols have redefined implant dentistry. The integration of 3D imaging, computer-guided surgery, and novel biomaterials reflects a continuous evolution toward enhancing predictability and success rates.
Latest advancements in implant technology for 2024
As we enter 2024, the landscape of implant dentistry boasts remarkable innovations. One notable advancement is the development of zirconia implants, which offer a tooth-colored alternative to traditional titanium. Their biocompatibility and aesthetic potential make them appealing options for specific clinical situations.
Additionally, the rise of digital dentistry has revolutionized treatment planning. Technologies like cone beam computed tomography (CBCT) allow practitioners to visualize complex anatomical structures, facilitating precise implant placement. Furthermore, 3D printing has emerged as a game-changer in producing custom surgical guides and prosthetics.
Another exciting trend is the use of surface modifications on implants. Enhanced surfaces that promote better osseointegration and reduce healing times are being engineered, resulting in improved outcomes. Biologically active coatings and nanostructured surfaces are becoming increasingly common, pushing the boundaries of what’s possible in implant success.
Anatomy and Physiology Relevant to Implant Dentistry
Understanding the anatomy and physiology relevant to implant dentistry is crucial for successful implant placement and long-term maintenance. This section will explore the key components of oral and maxillofacial anatomy and the biological processes underlying osseointegration.
Oral and maxillofacial anatomy for implant placement
A thorough grasp of oral and maxillofacial anatomy is paramount when planning and executing implant procedures. Key anatomical structures include the alveolar ridge, surrounding soft tissues, nerves, and blood vessels. A detailed anatomical map aids in avoiding complications and ensures proper implant positioning.
The alveolar ridge, which houses the roots of natural teeth, is a primary focus during implant placement. Variations in ridge shape and density can influence the choice of implant size, type, and placement technique. Knowledge of anatomical landmarks, such as the maxillary sinus and inferior alveolar nerve, is crucial for minimizing risks during surgery.
Additionally, the relationship between hard and soft tissues around the implants must be carefully considered. Adequate keratinized tissue is necessary to support long-term implant stability and aesthetics. An understanding of gingival biotype and its impact on peri-implant health is essential for achieving favorable outcomes.
Bone biology and osseointegration process
Osseointegration is the hallmark of successful dental implants. This phenomenon occurs when the implant fuses with the surrounding bone, creating a stable foundation for prosthetic teeth. It involves a complex interplay between biological processes and implant surface characteristics.
Bone healing begins immediately after implant placement, with a cascade of cellular events leading to new bone formation. Osteoblasts migrate to the implant surface, laying down a matrix that eventually mineralizes. The quality and quantity of bone play pivotal roles in the success of osseointegration; thus, assessing bone health before surgery is vital.
Emerging research highlights the significance of growth factors and stem cells in enhancing osseointegration. Techniques such as bone grafting and the use of bioactive materials are gaining traction, allowing for improved healing and integration of implants, even in challenging anatomical scenarios.
Patient Assessment and Treatment Planning for Implant Procedures

Thorough patient assessment and meticulous treatment planning are fundamental to successful implant outcomes. This section will discuss comprehensive evaluation techniques alongside the tools available for advanced imaging and planning.
Comprehensive patient evaluation techniques
A comprehensive patient evaluation encompasses a medical history review, clinical examination, and diagnostic tests. Understanding a patient’s systemic health is critical; conditions such as diabetes, osteoporosis, and autoimmune disorders can significantly affect healing and implant success.
During the clinical examination, factors such as oral hygiene, periodontal health, and occlusion must be assessed. A well-rounded evaluation helps identify any contraindications and enables personalized treatment planning.
Patient communication is equally important. Engaging patients in discussions about their expectations, concerns, and aesthetic preferences helps tailor treatment plans to meet individual needs. Establishing rapport fosters trust and collaboration, contributing to overall satisfaction.
Advanced imaging technologies in implant planning
Modern imaging technologies have revolutionized treatment planning in implant dentistry. Cone beam computed tomography (CBCT) provides high-resolution 3D images of the craniofacial complex, allowing practitioners to visualize anatomical structures with unprecedented clarity.
With CBCT, clinicians can assess bone volume and density accurately, facilitating informed decisions regarding implant size and position. Surgical guides developed from digital scans enhance precision during implant placement, reducing the risk of complications and improving outcomes.
Moreover, digital platforms allow for the creation of virtual treatment plans. Utilizing software to simulate the entire implant procedure empowers practitioners to predict potential challenges and address them proactively, streamlining the overall treatment process.
Implant Materials and Design: 2024 Update

Choosing the right materials and designs for dental implants is critical to long-term success. This section explores the latest developments in implant materials and design features that optimize integration and function.
Latest implant materials: Titanium vs. Zirconia
Titanium has long been recognized as the material of choice for dental implants due to its strength, biocompatibility, and osseointegration capabilities. However, zirconia implants are gaining popularity, particularly for patients seeking metal-free alternatives.
Zirconia offers aesthetic advantages with its tooth-colored appearance, making it an attractive option for anterior restorations. Research indicates that zirconia can achieve comparable osseointegration to titanium under certain conditions. Nevertheless, the mechanical properties and long-term performance of zirconia require careful evaluation based on the patient’s specific needs.
Ultimately, the choice between titanium and zirconia should be guided by patient preference, clinical indications, and evidence-based recommendations. Both materials have unique benefits and limitations, necessitating a comprehensive understanding of their applications.
Implant design features for optimal integration and function
Innovative implant designs are continuously emerging to enhance the functionality and longevity of dental implants. Thread patterns, platform switching, and surface treatments are just some design features that contribute to successful outcomes.
Thread design can influence initial stability and distribution of forces applied to the bone. Implants with tapered designs facilitate placement in compromised sites while maximizing primary stability. Platform switching, which involves placing a smaller abutment on a larger implant body, promotes crestal bone preservation.
Surface treatments play a significant role in osseointegration. Textured or coated surfaces can increase the contact area between the implant and bone, ultimately accelerating healing. The evolution of implant design emphasizes the importance of balancing mechanical resilience with biological compatibility.
Surgical Techniques in Implant Dentistry
The surgical phase is a critical component of implant dentistry, requiring skilled execution of protocols to ensure success. This section will cover basic and advanced implant placement techniques, along with digital workflows that enhance surgical precision.
Basic and advanced implant placement protocols
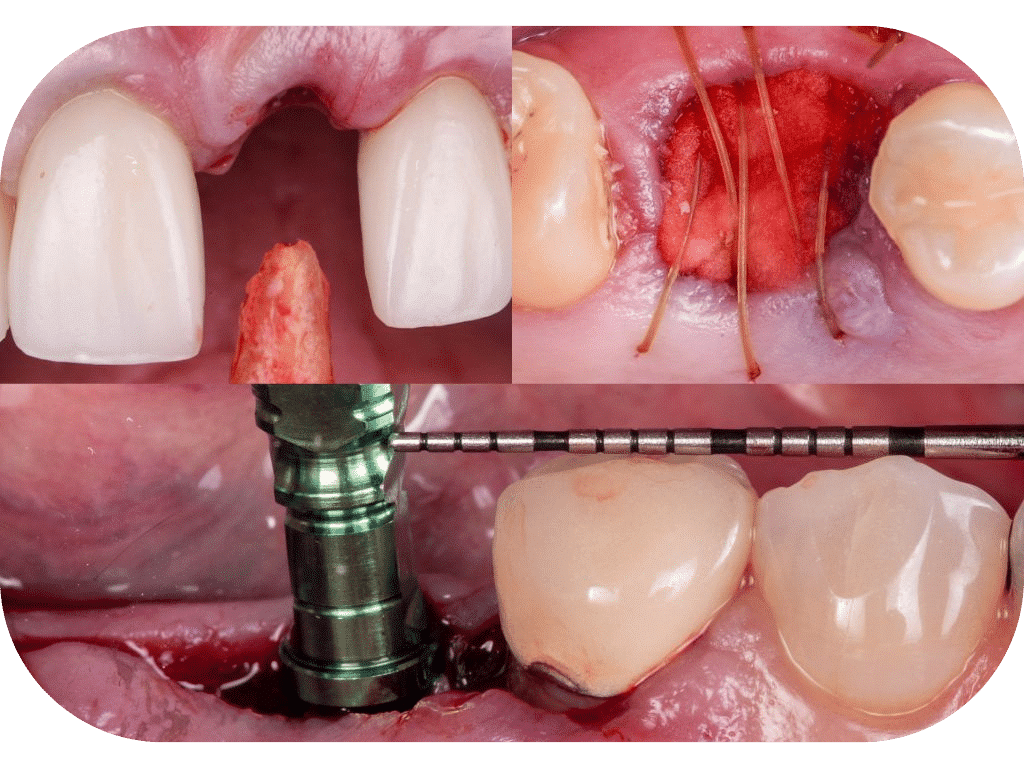
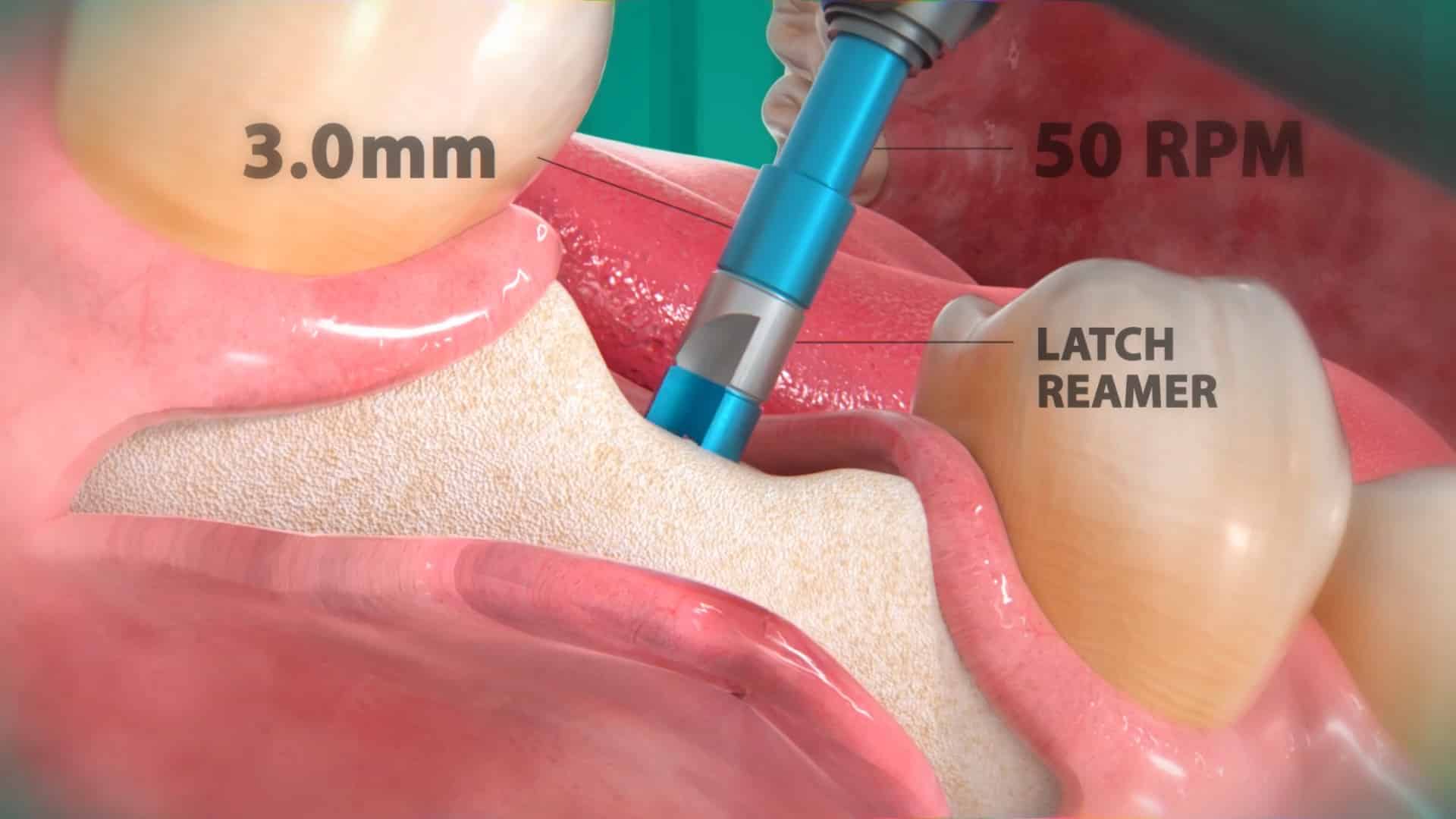
Basic implant placement protocols involve a straightforward sequence: site preparation, implant insertion, and post-operative care. However, implant dentists must tailor their approach to accommodate various clinical scenarios, including bone quality and quantity.
Advanced techniques, such as flapless surgery and immediate implant placement, are increasingly employed to minimize patient discomfort and recovery time. Flapless approaches rely on precise imaging and guided surgery, allowing for minimally invasive implantation while preserving soft tissues.
Furthermore, the concept of immediate loading—where the implant is loaded with a temporary crown on the same day as placement—requires careful case selection and adherence to strict criteria. Success depends on adequate primary stability and the absence of infection.
Guided implant surgery and digital workflows
Guided implant surgery represents a significant advancement in the field. With the use of digital impressions, surgical guides can be manufactured based on 3D imaging, allowing for highly accurate implant placement in predetermined positions.
This digital workflow enhances predictability, reducing the margin of error associated with freehand techniques. Practitioners can pre-plan the entire procedure, visualizing the final outcome before the first incision is made.
Additionally, incorporating virtual reality and augmented reality technologies into surgical training and practice is on the horizon. Such innovations promise to further elevate precision and confidence in implant placement.
Prosthetic Considerations in Implant Dentistry
Prosthetic planning is crucial for the overall success of dental implants. This section will discuss the types of implant-supported prostheses available and the fundamental principles of occlusion that must be considered.
Implant-supported prosthesis types and selection criteria
Various types of implant-supported prostheses are available, each designed to meet specific patient needs. Fixed prostheses, removable dentures, and hybrid options can all provide effective solutions for restoring function and aesthetics.
When selecting the appropriate prosthesis, factors such as the number of missing teeth, bone quality, and patient preferences are taken into account. Full arch restorations may utilize implant-supported fixed dentures to provide enhanced stability and comfort.
Collaboration between the oral surgeon and prosthodontist is essential for seamless integration of the prosthetic component. Interdisciplinary teamwork ensures that the aesthetics, function, and longevity of the final restoration are optimized.
Occlusion principles for implant-supported restorations
Understanding occlusion is key to the success of implant-supported restorations. The occlusal scheme must be balanced to avoid excessive forces on the implants and surrounding tissues. Ideal occlusion considers centric occlusion and dynamic occlusion, as both influence implant longevity.
Adjustments to occlusion may be necessary to prevent overload and premature failure. Proper articulation and alignment of opposing dentition are vital to establish a harmonious relationship that preserves the integrity of the implant and surrounding structures.
Furthermore, maintaining healthy peri-implant tissues through careful occlusal management is essential. Ensuring that the loading forces are distributed evenly contributes to the long-term success of the implant-supported restoration.
Soft and Hard Tissue Management in Implant Procedures
Effective management of both soft and hard tissues is essential for the success of implant procedures. This section will explore techniques to augment soft tissues and regenerate bone as needed.
Techniques for soft tissue augmentation around implants
Soft tissue augmentation techniques enhance the quantity and quality of soft tissues around implants. Sufficient keratinized tissue is necessary to support long-term stability and aesthetics.
Common techniques include connective tissue grafting and guided tissue regeneration. These methods can improve the volume and contour of the gingiva surrounding the implant site, facilitating better healing and aesthetic outcomes.
Utilizing biomaterials such as collagen membranes and xenografts expands the possibilities for soft tissue management. Advances in surgical techniques enable practitioners to achieve predictable results in augmenting tissues around implants.
Bone grafting and regeneration procedures in implantology
Bone grafting is often necessary for patients with insufficient alveolar bone to support an implant. Autogenous bone grafts, allografts, and synthetic bone substitutes offer diverse options for addressing bone deficiencies.
The choice of graft material depends on the defect’s location, size, and patient-specific factors. Guidance from radiographic evaluations and 3D imaging can aid in determining the most suitable approach.
Regenerative techniques, such as using growth factors and stem cell therapy, are gaining traction in implantology. These methods aim to enhance bone healing and regeneration, ultimately leading to more successful implant placements.
Immediate Loading Protocols and Their Applications
Immediate loading protocols represent a transformative approach to implant dentistry, allowing patients to receive functional restorations sooner. This section will detail the criteria for successful immediate loading and considerations for case selection.
Criteria for successful immediate loading
Immediate loading of implants requires specific criteria to ensure success. Primary stability is paramount—an implant must exhibit sufficient stability at the time of placement to withstand occlusal forces.
Other essential factors include the quality of the surrounding bone, the position of the implant, and careful assessment of the patient’s overall health. Rigorous case selection is critical; not every patient or situation is suitable for immediate loading.
Protocols must also account for the use of provisional restorations, which should be designed to minimize stress on the implant during the healing phase. A clear understanding of these criteria allows practitioners to confidently implement immediate loading protocols.
Case selection and treatment planning for immediate loading
Selecting appropriate cases for immediate loading requires a meticulous approach. Factors such as the number of implants, the presence of adjacent natural teeth, and the anticipated functional load must be evaluated.
Thorough treatment planning includes imaging studies to assess bone density and volume. Collaboration between the surgical and prosthetic teams ensures cohesive planning, allowing for a streamlined process from placement to restoration.
Clear communication with patients about the benefits and potential risks of immediate loading is also vital. Educating patients about postoperative care and maintenance contributes to overall satisfaction and successful outcomes.
Complications in Implant Dentistry: Prevention and Management
Complications can arise during or after implant procedures, affecting patient outcomes. This section will address common surgical and prosthetic complications, along with strategies for prevention and management.
Common surgical and prosthetic complications
Surgical complications may include implant failure, infection, or damage to adjacent anatomical structures. Preoperative assessments and careful surgical techniques can mitigate many of these risks.
Prosthetic complications can arise during the fabrication or fitting of the restoration. Issues such as inadequate occlusion, aesthetic discrepancies, and mechanical failure must be identified and addressed promptly.
Ongoing monitoring and maintenance of implants are essential to preventing complications. Regular follow-ups enable practitioners to detect potential issues and intervene before they escalate.
Peri-implantitis: Diagnosis, prevention, and treatment
Peri-implantitis is a significant concern in implant dentistry, characterized by inflammation and bone loss around an implant. Early diagnosis is critical for effective management, so practitioners must be vigilant in monitoring peri-implant tissues.
Prevention strategies include educating patients on oral hygiene practices and regular professional cleanings. Maintaining a healthy peri-implant environment is vital for long-term success.
Treatment options range from non-surgical interventions to surgical revision, depending on the severity of the condition. A customized treatment approach tailored to the individual patient’s needs provides the best chance for resolution.
Future Trends in Implant Dentistry for 2024 and Beyond
As implant dentistry continues to evolve, new trends and technologies emerge, shaping the future of the field. This section will explore the promising advancements that are set to redefine implant practices in the coming years.
Emerging technologies in implant dentistry
Technological advancements are playing a pivotal role in enhancing the efficacy of implant dentistry. Virtual reality and augmented reality are beginning to find applications in surgical training and procedure planning, improving visualization and precision.
Artificial intelligence is also making waves, with algorithms being developed to assist in diagnostics, treatment planning, and predicting outcomes. The incorporation of AI can lead to greater accuracy and efficiency in managing complex cases.
Moreover, tele-dentistry provides opportunities for remote consultations and follow-up care, allowing for increased accessibility and convenience for patients and providers alike.
The role of AI and robotics in implant procedures
Robotics is poised to transform surgical techniques in implant dentistry. Robotic-assisted systems can enhance the precision of implant placement, reducing the potential for human error and increasing consistency across procedures.
AI-powered software can analyze vast amounts of data, helping clinicians make informed decisions and streamline workflows. As these technologies continue to develop, they hold the potential to improve patient experiences and outcomes significantly.
Integrating AI and robotics into everyday practice will demand investment in training and resources. However, the potential benefits, including improved accuracy, reduced surgical times, and enhanced patient satisfaction, make this transition worthwhile.
Integrating Implant Dentistry into Your Practice
Successfully integrating implant dentistry into a dental practice requires thoughtful planning and execution. This section will outline the steps necessary to build a skilled implant team and effectively market implant services.
Building a skilled implant team
Establishing a skilled implant team is essential for delivering high-quality care. This team typically consists of oral surgeons, periodontists, prosthodontists, and dental hygienists, each playing a vital role in the implant process.
Continuing education is critical for staying updated on advancements in implant techniques and technologies. Encouraging team members to pursue additional training and certifications enhances overall competence within the practice.
Fostering a culture of collaboration and communication among team members streamlines workflows and enriches the patient experience. Regular team meetings and case reviews promote knowledge sharing and strategic planning.
Marketing implant services effectively
Marketing implant services requires a multi-faceted approach. Educating the public about the benefits of dental implants is essential for attracting potential patients.
Creating engaging content through blogs, social media, and local outreach can raise awareness and foster trust. Showcasing before-and-after photos of successful cases and sharing patient testimonials can also enhance credibility.
Collaborating with local general dentists and specialists can lead to referral partnerships, broadening the reach of implant services. Hosting community events to educate the public on oral health and implant options can cultivate interest and generate leads.
Common Pitfalls to Avoid in Implant Dentistry
Despite the advances in implant dentistry, certain pitfalls can undermine the success of procedures. This section will highlight common mistakes and provide insights on how to avoid them.
Inadequate treatment planning
Inadequate treatment planning is one of the most significant pitfalls in implant dentistry. Rushing into procedures without thorough assessments can lead to complications and poor outcomes.
Taking the time to conduct comprehensive evaluations, including medical history, imaging studies, and patient preferences, is critical. Meticulous planning sets the stage for successful implant placement and restoration.
Overlooking patient’s systemic health conditions
Ignoring a patient’s systemic health conditions can jeopardize the success of implants. Conditions such as uncontrolled diabetes, cardiovascular disease, and smoking habits can negatively impact healing and osseointegration.
Practitioners must engage in open dialogue with patients about their health status and collaborate with medical professionals when needed. Comprehensive patient care encompasses addressing systemic health factors alongside dental treatment.
Frequently Asked Questions
What are the success rates of dental implants in 2024?
Success rates of dental implants remain high in 2024, with studies reporting over 90% success rates for single-tooth implants. Factors such as bone quality, patient compliance, and maintenance of oral hygiene play pivotal roles in achieving optimal outcomes.
How long does the entire implant process typically take?
The timeline for the implant process varies based on individual circumstances. Generally, the process spans several months, including healing periods post-placement. Immediate loading techniques can expedite restoration timelines for select patients.
Are there any new alternatives to traditional dental implants in 2024?
While traditional dental implants remain the mainstay of tooth replacement, advancements in biomaterials, mini implants, and innovative prosthetic designs are emerging as promising alternatives for specific clinical situations.
What advancements have been made in implant surface technology?
Recent advancements in implant surface technology focus on enhancing osseointegration. Innovations include the development of nanoscale surface textures, bioactive coatings, and surface treatments that promote faster healing and improved stability.
How has digital dentistry improved implant procedures?
Digital dentistry has revolutionized implant procedures by enabling precise diagnostics, treatment planning, and implant placement. Tools such as 3D imaging, computer-guided surgery, and virtual simulations enhance accuracy and predictability.
Conclusion
The fundamentals of implant dentistry 2024 underscore the dynamic nature of this field, reflecting ongoing advancements in technology and techniques. By understanding the historical context, honing anatomical knowledge, implementing robust assessment protocols, selecting optimal materials, executing precise surgical techniques, and embracing innovative approaches, dental professionals can significantly improve patient outcomes.
As we look toward the future, staying abreast of emerging trends, embracing new technologies, and fostering interdisciplinary collaborations will be vital for continued success in implant dentistry. Ultimately, the goal remains clear: to provide patients with functional, aesthetically pleasing restorations that restore confidence and enhance quality of life.