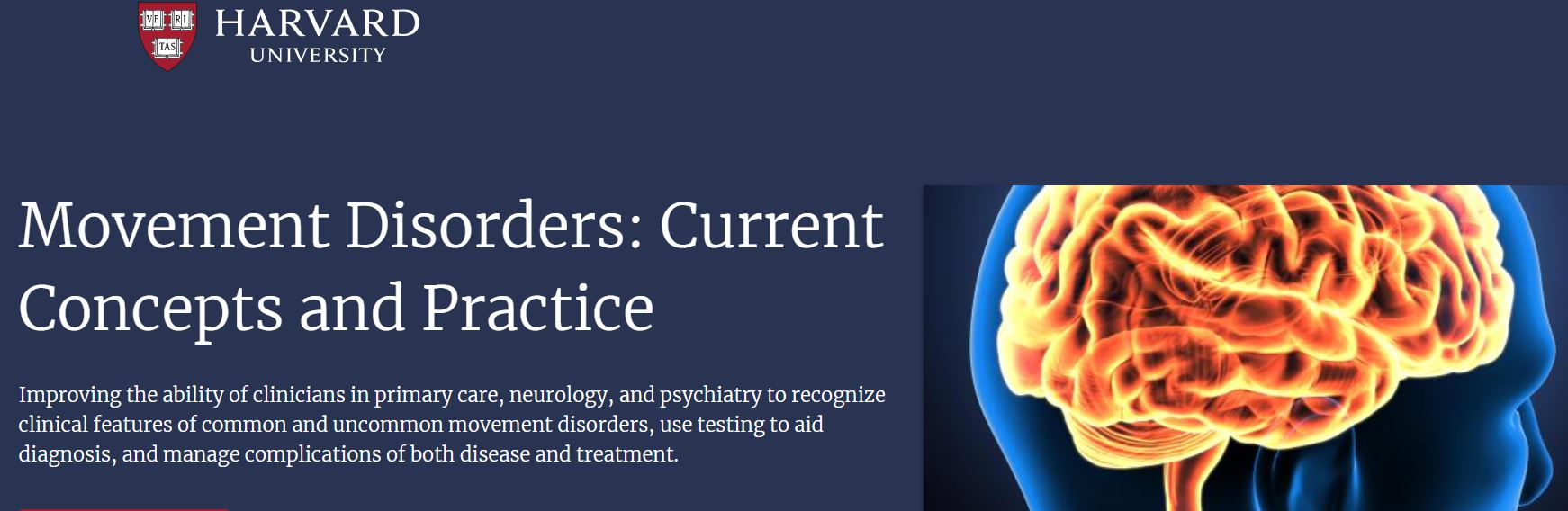
Harvard Movement Disorders – Current Concepts And Practice 2023 (Videos Only)
150 $
Format : 34 MP4 files
File Size : 5.71 GB
Course Overview
The goal of this course is to improve the ability of clinicians in primary care, neurology, and psychiatry to recognize clinical features of common and uncommon movement disorders, use testing to aid diagnosis, and manage complications of both disease and treatment. The evaluation and management of movement disorders depends upon targeted, historical assessment and physical examination of the patient. Conditions, such as essential tremor and Parkinson’s disease, are common and can produce significant disability and disease burden on patients and their caregivers.
Though Parkinson’s disease and essential tremor are two well-known disorders commonly encountered by the general practitioner and neurologist, a considerable percentage of cases are misdiagnosed. In addition, other highly treatable disorders, such as drug-induced movement disorders, dystonia, and tics can be difficult to recognize which can pose an obstacle to initiating proper treatment. There have been considerable advances in our understanding of certain complex movement disorders, such as Parkinson’s disease. We will also focus attention on non-motor aspects of Parkinson’s disease, which are increasingly being recognized as important determinants of quality of life.
The course will cover current concepts on pathophysiology of the various movement disorders, evidence-based evaluation and treatment recommendations, clinical practice guidelines as well as experience-based recommendations. Numerous patient videos will be shown throughout the presentations. Finally, the course will culminate with interactive discussion of video-based case examples.
Who Should Attend
Primary Care Physicians
Nurses
Nurse Practitioner
Other
Primary Care Practitioner
Pharmacists
Specialty Physicians,
Physician Assistant
Psychologists
Movement Disorder Fellows
Learning Objectives
Upon completion of this activity, participants will be able to:
Evaluate and diagnose movement disorders, such as Parkinson’s disease, Huntington’s disease, dystonia, tremor, myoclonus, tics, gait disturbances, chorea, tardive dyskinesia, and other disorders of the basal ganglia, in different settings (emergency, inpatient, and outpatient).
Summarize treatment options and considerations in the management of movement disorders.
Recognize pitfalls in making an erroneous diagnosis in Parkinson’s disease, tremor or dystonia.
Describe the pharmacology and side effects of commonly used medications for treatment of various movement disorders.
Interpret the role of dopamine blockers in disease pathophysiology and management of tardive dyskinesia and drug-induced parkinsonism.
Integrate physical examination techniques into practice to aid in the diagnosis of a movement disorder.
Summarize diagnostic criteria and genetic counseling principles necessary for evaluating patients with suspected hereditary chorea or ataxia.
Explain a clinical evaluation method for gait disorders as well as diagnostic “red flags” that aid in the diagnosis of atypical parkinsonism.
Identify relevant components of the basic anatomy and pathophysiology of the basal ganglia as it pertains to movement disorders.
Assess potential therapeutic uses of botulinum toxin injections for dystonia, hemifacial spasm, and related disorders.
Discuss patient factors in the screening of candidates for deep brain stimulation.
Identify relevant issues regarding pre-operative evaluation and post-operative care for patients receiving deep brain stimulation.
Examine physical examination techniques and history taking skills in making the diagnosis of a psychogenic movement disorder.
Describe common non-motor aspects of Parkinson’s disease, including mood disorders and cognitive impairment, and summarize treatment options and best practices.
Be the first to review “Harvard Movement Disorders – Current Concepts And Practice 2023 (Videos Only)” Cancel reply
You must be logged in to post a review.
Related Products
Medical Book
Medical Book
Medical Book










Reviews
There are no reviews yet.